SPECIALIZATIONS
Interventional pulmonology is a safe and noninvasive way to diagnose and treat lung disorders. Our interventional pulmonologists specialize in all pulmonary diseases and complicated problems of the airways. Patients with lung cancer, cancer of the airways, pulmonary nodules, complex airways disease, complicated asthma, and other pulmonary conditions will benefit from our full scope of advanced services. For patients with early endobronchial disease or the most complex lung condition, we offer every diagnostic and therapeutic modality available.
Interventional Pulmonology Procedures
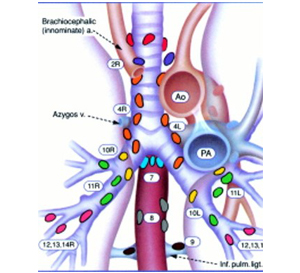
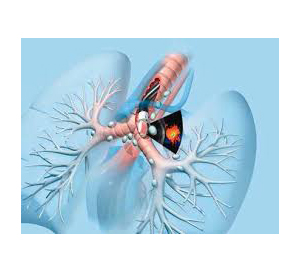
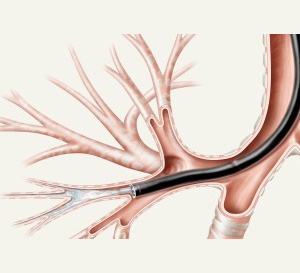
Endobronchial ultrasound (EBUS) is a technique that uses ultrasound along with bronchoscope to visualize mediastinal lymph nodes and lung nodules. It is minimally invasive technology & highly effective procedure to sample mediastinal & hilar nodes for diagnosis such as:
- Investigate enlarged lymph nodes in the chest.
- Diagnose conditions such as sarcoidosis or tuberculosis.
- Diagnose & Stage Cancer
What are mediastinal & hilar lymph nodes?
Mediastinal & hilar lymph nodes are anatomic structures that play an important role the body's lymphatic system. They are located in a region of the body called the mediastinum, which is part of the chest cavity between the heart and lungs.
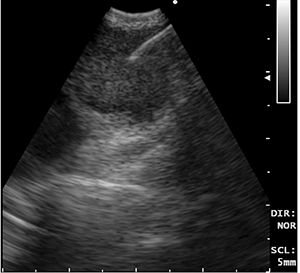
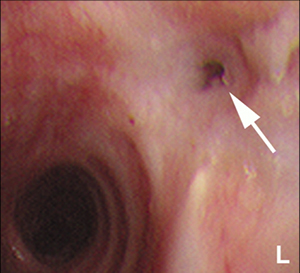
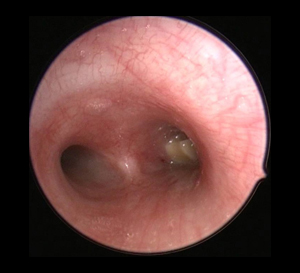
What is EBUS TBNA?
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) is a reliable and an established technique, which can be perceived as the current gold standard that enables visualisation and sampling of mediastinal or hilar lymph nodes under real time ultrasound guidance.
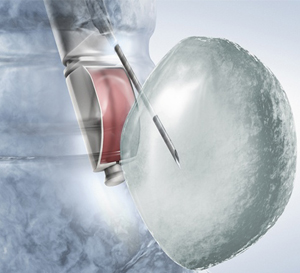

How is EBUS TBNA performed?
EBUS TBNA procedure is most often performed under local anaesthesia and sedation on day care basis. Sometimes patients may need to be hospitalised.
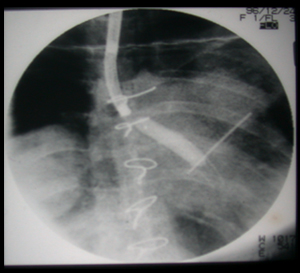
The dedicated EBUS TBNA broncoscope is passed orally through the vocal cords into the airway. The mediastinal and hilar lymph nodes are visualised on the monitors using the ultrasound probe at the tip of bronchoscope. The EBUS-TBNA needle is inserted into the lymph nodes under real time ultra sound guidance and samples obtained.
What are the chances of making the diagnosis?
The diagnosis yield on EBUS –TBNA may vary from 74% to 95%. In our recently published scientific paper, the diagnostic yield in our setting was 89%.
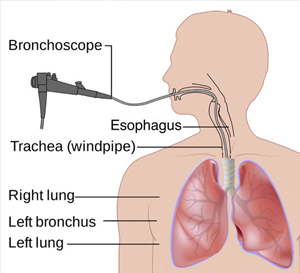
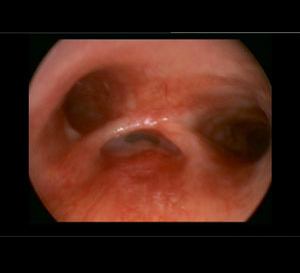
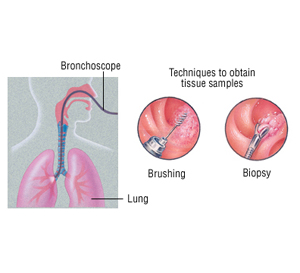
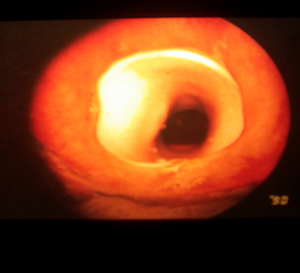
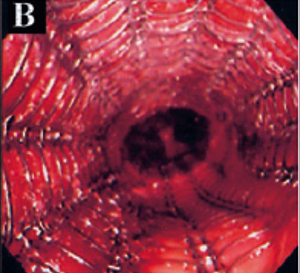
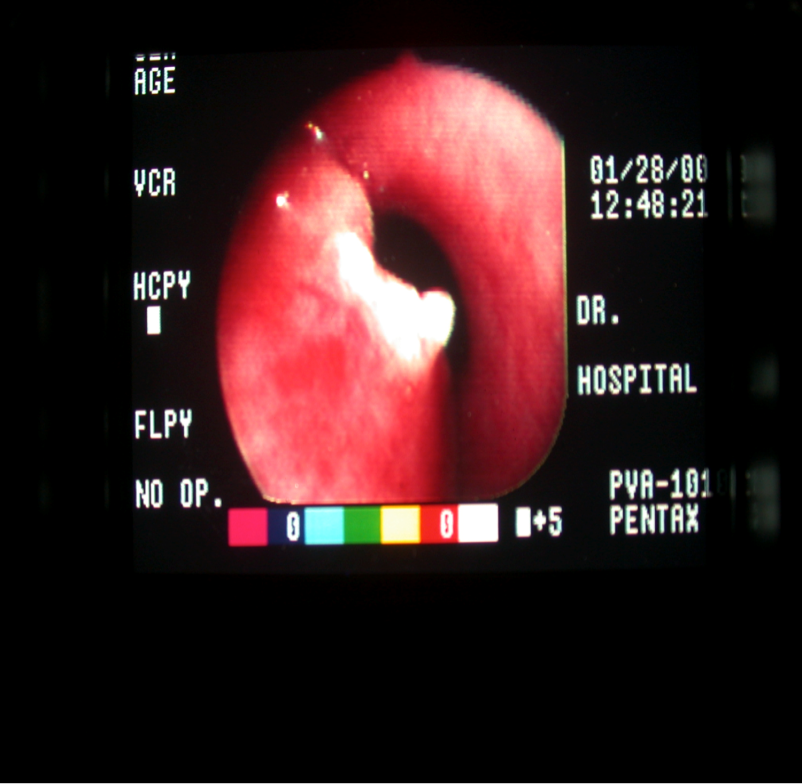
Bronchoscopy is the most common interventional pulmonology procedure. During bronchoscopy, a doctor advances a flexible endoscope (bronchoscope) through a person's mouth or nose into the windpipe. The doctor advances the bronchoscope through the airways in each lung, checking for problems. Images from inside the lung are displayed on a video screen.
The bronchoscope has a channel at its tip, through which a doctor can pass small tools. Using these tools, the doctor can perform several other interventional pulmonology procedures.
Bronchoalveolar lavage is performed during bronchoscopy. Sterile water is injected through the bronchoscope into a segment of the lung. The fluid is then suctioned back and sent for tests. Bronchoalveolar lavage can help diagnose infection, cancer, bleeding, and other conditions.
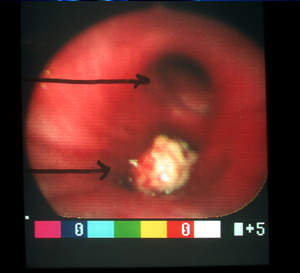

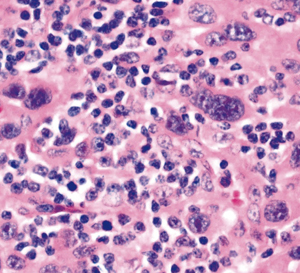
During bronchoscopy, a doctor may collect a small piece of tissue from either the lung or a nearby lymph node. The interventional pulmonologist can use a needle or forceps advanced through the bronchoscope to get a sample of tissue. Biopsies can detect cancer, infection, sarcoidosis, and other conditions.
For people with lung cancer or other cancers, interventional pulmonology biopsies can often accurately identify spread of cancer into lymph nodes. This can prevent unnecessary surgery or help determine the best choice for treatment.
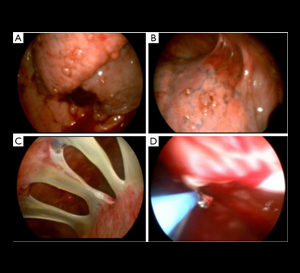
Advanced cancer or certain other conditions can constrict or compress an airway tube (bronchus). If the bronchus becomes blocked, difficulty breathing, cough, and pneumonia can result.
Using a bronchoscope, a doctor can advance a wire mesh stent into a narrowed airway. Expanding the stent can open a bronchus and relieve symptoms caused by the constriction.
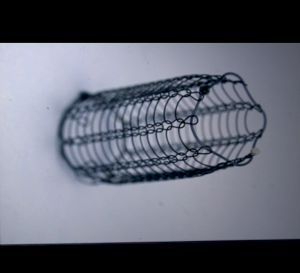
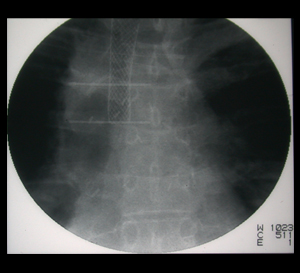
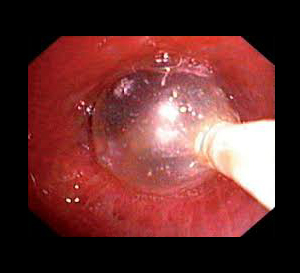
A doctor advances a deflated balloon into a section of abnormally narrowed airway. By inflating the balloon with water, the airway is expanded, potentially relieving symptoms. Balloon bronchoplasty may be performed prior to airway stent placement to help expand a bronchus.
In rigid bronchoscopy, a long metal tube (rigid bronchoscope) is advanced into a person’s windpipe and main airways. The rigid bronchoscope’s large diameter allows the doctor to use more sophisticated surgical tools and techniques. Rigid bronchoscopy requires general anesthesia (unconsciousness with assisted breathing), similar to a surgical procedure.

Bronchoscopy is the preferred interventional pulmonology procedure to remove inhaled foreign objects that are lodged in an airway. A doctor may be able to remove the object using flexible bronchoscopy, or rigid bronchoscopy may be required.
A doctor cuts small incisions in the chest wall and advances a pleuroscope (a type of endoscope) into the chest cavity. The pleuroscope is advanced around the chest wall and lung on one side. Pleuroscopy can diagnose some conditions of the pleura (lining of the lung). Pleuroscopy also allows a view of the outside edges of the lung, which bronchoscopy cannot provide.
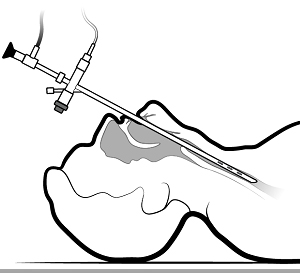
To drain fluid from around the lungs (pleural effusion), a doctor inserts a needle into the chest wall. A plastic catheter is advanced over the needle, which is then removed. The excess pleural fluid is suctioned out of the chest and the catheter is removed and discarded.
Pleurodesis is an interventional pulmonology procedure performed for people with recurring pleural effusions (fluid around the lungs). In pleurodesis, a doctor makes an incision in the chest wall. A plastic tube is inserted into the chest cavity, and an irritating chemical is sprayed around the lung. Over time, the inflamed lung lining (pleura) adheres tightly to the chest wall. This prevents fluid from reaccumulating around the lung.
In obstructive sleep apnea the upper airway repeatedly collapses during sleep, causing a decreased airflow that stresses the heart, the body and raises blood pressure. this condition may worsen glucose control and insulin resistance, and lead to blood sugar imbalance. for some people, their airflow decreases during sleep which causes sleep disruptions and decreased sleep quality. sleep disordered breathing may cause daytime sleepiness, headaches, lack of energy and chronic aches and paions.
Obstructive sleep apnea is a common disorder in which the patient has one or more pauses in breathing or shallow breaths while sleeping. people who have obstructive sleep apnea stop breathing repeatedly during sleep because the airway collapses. as a result,air is prevented from getting into the lungs & reduces the oxygen in the blood.
| Normal Breathing | Obstructive Sleep Arena |
 |
 |
- Snoring
- Day time fatigue and sleepiness
- Sleepiness while watching tv or reading
- Morning headaches
- Urination at night
- A dry throat on waking up
- Gasping or choking at night
- Teeth grinding
- Disrupted sleep
- Night time arm and leg movements
- High blood pressure
- Heart failure
- Stroke
- Obesity
- Diabetes
- Increase risk of having work related or driving accidents
- Mood swings
- Irritability
- Poor memory, learning problems or inability to concentrate
- Personality changes
- Panic attacks
Clinical studies have shown a link between the following medical conditions and obstructive sleep apnea (OSA).
- High blood pressure
- Stroke
- Type II diabetes
- Chronic pain syndrome
- Insomania
- Women who have gone through menopause
In order to be properly diagnosed, an overnight test is undertaken where sleep patterns, breathing and heart activity are monitored and recorded. the overnight recording is safe and painless.
Clinical studies have shown that treatment of OSA may
- Prevent or delay the progression of Type 2 diabetes
- Reduce diabetic complications
- Improve daytime energy and glucose control
- Reduce the potential risk for heart attack, stroke and heart disease
 +91 9920095988
+91 9920095988